Central Sterile Services Department: Essential Healthcare Hub
Posted by Admin | 12 Feb
The Central Sterile Services Department (CSSD), also known as Central Sterile Supply Department or Sterile Processing Department (SPD), is a specialized hospital unit responsible for decontaminating, processing, sterilizing, and distributing reusable medical equipment and surgical instruments. This critical department ensures that all medical devices used in patient care are properly cleaned, inspected, packaged, and sterilized to prevent healthcare-associated infections and maintain patient safety across surgical suites, emergency departments, and clinical units.
Core Functions and Workflow
The CSSD operates through a precisely defined workflow divided into distinct zones to prevent cross-contamination. Each zone serves a specific purpose in the sterilization cycle, with staff moving instruments through a unidirectional flow from contaminated to sterile areas.
Decontamination Zone
This area receives contaminated instruments from operating rooms and clinical departments. Staff wearing appropriate personal protective equipment perform initial cleaning using:
- Ultrasonic cleaners that use high-frequency sound waves to remove debris from intricate instrument surfaces
- Automated washer-disinfectors operating at temperatures between 93°C and 95°C
- Enzymatic detergents specifically formulated to break down organic material
Inspection and Assembly Area
After decontamination, technicians meticulously inspect each instrument for functionality, cleanliness, and damage. Instruments are assembled into procedure-specific trays according to standardized picking lists. Studies indicate that proper inspection reduces surgical delays by up to 35% by ensuring all necessary instruments are functional and available.
Sterilization Processing
Multiple sterilization methods are employed based on instrument materials and heat sensitivity:
- Steam sterilization (autoclaving): Most common method, using saturated steam at 121°C-134°C for 3-30 minutes
- Ethylene oxide (EtO): Low-temperature process for heat-sensitive items, requiring 12-16 hours including aeration
- Hydrogen peroxide plasma: Modern alternative for delicate electronics and optics, completing cycles in 28-75 minutes
Quality Assurance and Monitoring
CSSD departments implement rigorous quality control measures to validate sterilization effectiveness. Each sterilization cycle undergoes multiple levels of monitoring to ensure patient safety.
| Monitoring Type | Method | Frequency | Purpose |
|---|---|---|---|
| Physical | Temperature, pressure, time gauges | Every cycle | Verify proper operating parameters |
| Chemical | Indicator strips/tape | Every package | Confirm exposure to sterilant |
| Biological | Spore tests (Geobacillus) | Daily/weekly | Validate microbial kill effectiveness |
Research from the Association for the Advancement of Medical Instrumentation (AAMI) demonstrates that facilities implementing comprehensive monitoring protocols experience 89% fewer sterilization failures compared to those using minimal oversight.
Regulatory Standards and Compliance
CSSD operations are governed by multiple regulatory bodies and professional organizations that establish processing standards. Compliance with these guidelines is mandatory for healthcare facility accreditation and patient safety certification.
Key Regulatory Frameworks
- AAMI ST79: Comprehensive guide to steam sterilization and sterility assurance in healthcare facilities
- ISO 17665: International standard for moist heat sterilization validation and routine control
- Joint Commission standards: Requirements for infection prevention and instrument processing
- CDC guidelines: Evidence-based recommendations for disinfection and sterilization in healthcare settings
Non-compliance can result in serious consequences. In 2023, the Joint Commission cited instrument processing deficiencies in 42% of surveyed hospitals, with violations ranging from inadequate documentation to improper storage of sterile items.
Staffing and Certification Requirements
CSSD personnel require specialized training and certification to properly execute sterile processing procedures. The complexity of modern surgical instruments and sterilization technologies demands ongoing education and competency assessment.
Professional Certification Programs
Several organizations offer nationally recognized credentials for sterile processing technicians:
- CRCST (Certified Registered Central Service Technician): Offered by HSPA, requiring 400 hours of hands-on experience
- CSPDT (Certified Sterile Processing and Distribution Technician): CBSPD certification with comprehensive examination
- CHL (Certified Healthcare Leader): Advanced credential for supervisory positions
Healthcare facilities with 80% or higher certification rates among CSSD staff report 56% fewer processing errors and demonstrate significantly improved surgical outcomes according to data from the Healthcare Sterile Processing Association.
Technology and Automation Advances
Modern CSSD departments increasingly incorporate advanced technologies to improve efficiency, traceability, and error reduction. These innovations transform traditional manual processes into sophisticated automated systems.
Instrument Tracking Systems
RFID (Radio Frequency Identification) and barcode technologies enable real-time tracking of instruments throughout the processing cycle. These systems provide:
- Complete instrument history from decontamination through patient use
- Automatic lot recall capabilities if sterilization failure is detected
- Usage analytics to optimize inventory and identify missing instruments
- Regulatory compliance documentation with complete audit trails
Implementation of tracking systems reduces instrument loss by 73% on average and decreases case delays due to missing instruments by 62%, according to peer-reviewed studies in healthcare management journals.
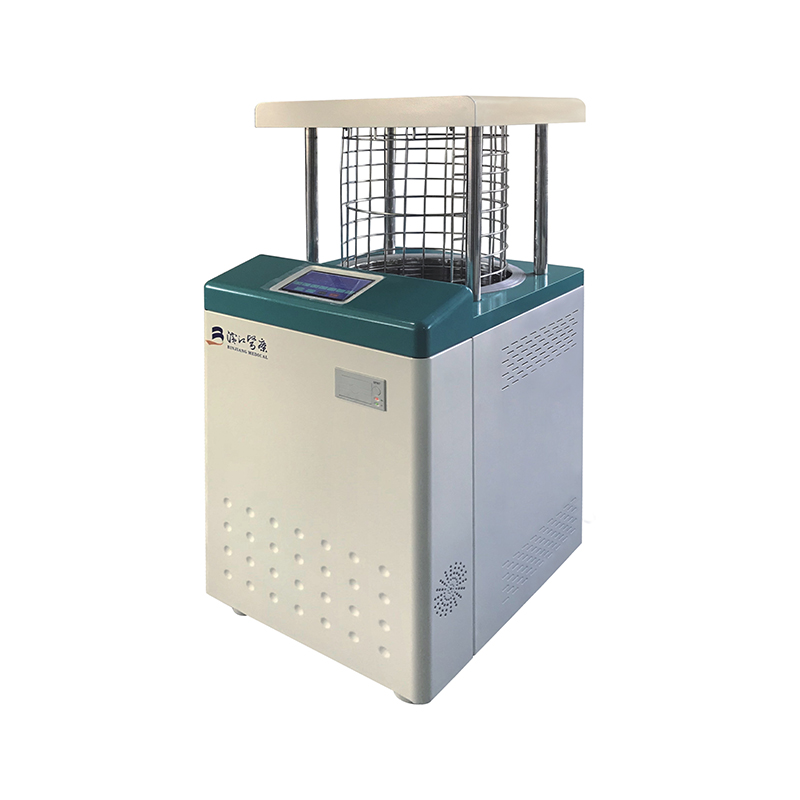
Automated Cleaning and Sterilization Equipment
Next-generation equipment features integrated monitoring, automated documentation, and connectivity to hospital information systems. Advanced washer-disinfectors now include chemical dispensing validation, water quality monitoring, and automated cycle selection based on instrument type recognition.
Impact on Patient Safety and Infection Prevention
The CSSD serves as a cornerstone of hospital infection control programs. Properly processed instruments directly prevent surgical site infections (SSIs) and device-related complications that can result in extended hospital stays, additional procedures, and increased mortality risk.
Centers for Disease Control and Prevention data indicates that surgical site infections affect approximately 2-5% of surgical patients annually, with significant portions attributable to inadequate instrument processing. A single SSI adds an average of $20,000-$30,000 in treatment costs and extends hospital stays by 7-10 days.
Critical Control Points
- Immediate instrument retrieval: Contaminated instruments should reach CSSD within 30-60 minutes to prevent biofilm formation
- Point-of-use treatment: Wiping instruments with enzymatic foam at the surgical field prevents protein coagulation
- Validated cleaning processes: Automated washers must undergo quarterly performance qualification testing
- Proper packaging: Maintaining package integrity until use ensures sterility is preserved for shelf-life duration
Challenges and Future Directions
Contemporary CSSD departments face evolving challenges including increasingly complex surgical instruments, workforce shortages, and rising operational costs. The introduction of robotic surgical systems with specialized cleaning requirements and single-use device reprocessing controversies add layers of complexity to traditional operations.
Workforce Development
The sterile processing field experiences annual turnover rates averaging 25-35%, creating continuity challenges and increasing training costs. Facilities are addressing this through:
- Career ladder programs offering advancement from technician to specialist to supervisor roles
- Competitive compensation packages recognizing the technical expertise required
- Partnerships with vocational schools to establish dedicated training programs
- Investment in simulation-based training for complex instrument processing
Sustainability Initiatives
Environmental considerations are driving CSSD departments toward sustainable practices without compromising sterility. Water recycling systems, energy-efficient sterilizers, and reusable packaging materials reduce environmental impact while maintaining regulatory compliance. Some facilities report reducing water consumption by 40% and energy use by 30% through equipment upgrades and process optimization.
Outsourcing and Centralization Trends
Healthcare systems are increasingly evaluating centralized sterile processing models where multiple facilities share a regional CSSD. This approach offers economies of scale, standardized processes, and specialized expertise concentration. However, logistics challenges, transportation considerations, and emergency case flexibility require careful planning.
A study of 15 healthcare systems implementing centralized processing found average cost reductions of 18-22% while maintaining or improving quality metrics. The model works best for high-volume standardized instrument sets, while specialized or emergency instruments often remain at individual facilities.
Third-party reprocessing companies also offer outsourcing options for specific instrument categories, particularly complex scopes and powered surgical devices requiring specialized equipment and expertise. Approximately 35% of US hospitals now utilize some form of outsourced sterile processing services according to industry surveys.

 English
English русский
русский Français
Français Español
Español bahasa Indonesia
bahasa Indonesia Deutsch
Deutsch عربى
عربى 中文简体
中文简体