EO Sterilization Process: Comprehensive Guide for Medical Device Safety
Posted by Admin | 23 Oct
1. Introduction to EO Sterilization Process
Ethylene oxide (EO) sterilization is a widely used method for sterilizing heat-sensitive medical devices and instruments. Unlike steam sterilization, EO uses a chemical process that effectively eliminates bacteria, viruses, and fungi without damaging delicate equipment. It is especially important in the healthcare and pharmaceutical industries where maintaining product sterility is critical.
2. Principle of EO Sterilization
The EO sterilization process relies on the alkylation of microbial DNA and proteins by ethylene oxide gas. This reaction inhibits cellular reproduction and metabolic functions, effectively killing microorganisms. The process is carried out under controlled temperature, humidity, and gas concentration to ensure complete sterilization.
3. Key Stages of EO Sterilization
3.1 Preconditioning
Medical devices are exposed to controlled temperature and humidity to prepare them for the EO sterilization process. Preconditioning ensures that the EO gas can penetrate all surfaces, including complex device geometries and packaging materials.
3.2 EO Gas Exposure
Devices are placed in a sterilization chamber where EO gas is introduced. The exposure time depends on the product type, chamber size, and required sterility assurance level (SAL). Typical exposure times range from 2 to 12 hours at temperatures between 37°C and 63°C.
3.3 Aeration
After sterilization, residual EO gas is removed from the devices through aeration. This stage is critical for safety, as EO is toxic and flammable. Aeration may take several hours to several days depending on the device material and packaging.
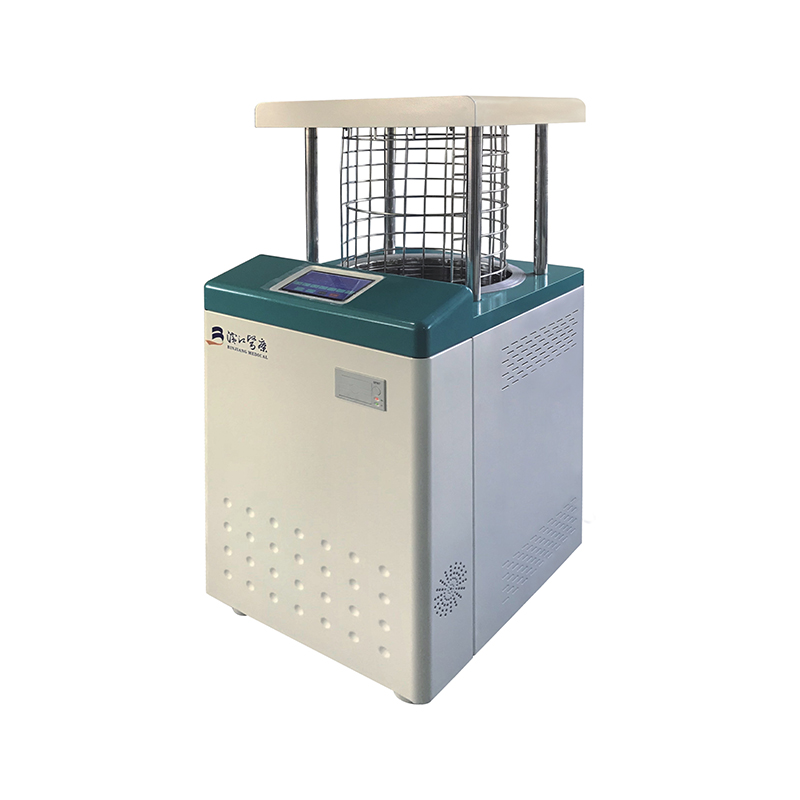
4. Equipment and Materials Used in EO Sterilization
Successful EO sterilization requires specialized equipment and monitoring tools. Commonly used items include:
- Ethylene oxide sterilizer chamber with temperature and humidity control
- Gas injection and circulation systems
- Biological indicators to validate sterilization
- Monitoring sensors for EO concentration and exposure time
- Aeration cabinets or controlled airflow systems for residual gas removal
5. Applications of EO Sterilization
EO sterilization is ideal for items that cannot withstand high temperatures or moisture. Typical applications include:
- Plastic syringes, catheters, and tubing
- Electronic medical devices
- Implants and prosthetics
- Pharmaceutical packaging
- Disposable medical instruments
6. Advantages and Limitations of EO Sterilization
6.1 Advantages
- Effective at low temperatures, suitable for heat-sensitive devices
- Can penetrate complex devices and packaging
- High sterility assurance level achievable
- Minimal impact on device functionality and material integrity
6.2 Limitations
- Residual EO can be toxic; thorough aeration is necessary
- Long sterilization and aeration cycles compared to other methods
- Specialized equipment and trained personnel required
- Strict regulatory and safety compliance needed
7. Safety and Regulatory Considerations
EO sterilization must comply with regulatory standards such as ISO 11135 and FDA guidelines. Key safety measures include:
- Continuous monitoring of EO levels in sterilization and aeration areas
- Proper personal protective equipment (PPE) for operators
- Validation of sterilization cycles using biological indicators
- Safe storage and handling of EO gas cylinders
8. Conclusion
The EO sterilization process remains an essential method for sterilizing heat-sensitive and complex medical devices. Understanding its principles, procedures, equipment requirements, and safety measures ensures effective sterilization while maintaining device integrity and patient safety. Careful adherence to regulatory standards and process validation is key to maximizing the benefits of EO sterilization.

 English
English русский
русский Français
Français Español
Español bahasa Indonesia
bahasa Indonesia Deutsch
Deutsch عربى
عربى 中文简体
中文简体