Frequently Asked Questions about Sterilization Supply Center
Posted by Admin | 17 Sep
1.Basic concepts of medical sterilization supply center
Medical Sterilization and Supply Center
The Medical Sterilization and Supply Center is primarily responsible for the cleaning, disinfection, and sterilization of reusable medical instruments, instruments, clean surgical gowns, drapes, and other items for medical institutions, as well as the supply of sterile supplies. The center also conducts quality control throughout the processing process, issues monitoring and testing results, and ensures full traceability and quality assurance.

Standard Precautions
A patient's blood, body fluids, secretions, and excretions are deemed infectious and must be isolated. Regardless of whether there is obvious blood contamination or contact with non-intact skin or mucous membranes, all individuals who come into contact with these substances must take preventive measures.
Decontamination
The process of removing organic and inorganic matter and microorganisms from handled items.
Cleaning
The complete process of removing contaminants from medical devices, instruments, and items, including rinsing, washing, rinsing, and a final rinse.
Disinfection
The process of killing or eliminating pathogenic microorganisms on a transmission medium, rendering it harmless. However, bacterial spores cannot be killed.
Sterilization
The process of killing or eliminating all microorganisms (including bacterial spores) on a transmission medium.
Wet Heat Disinfection
The process of using moist heat to denature bacterial proteins or inactivate coagulase, disrupting metabolism, and causing cell death. Examples include boiling, pasteurization, and low-temperature steam sterilization.
Sterilization Process Validation Device
A simulated device with a predetermined resistance to the sterilization process, used to evaluate the effectiveness of the sterilization process. When a chemical indicator is placed inside, it is called a chemical PCD; when a biological indicator is placed, it is called a biological PCD.
A0 Value
An indicator for evaluating the effectiveness of moist heat disinfection. It refers to the time (in seconds) that a temperature of 80°C is maintained when the microbial killing effect, expressed as a Z value, is 10K.
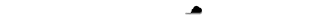
Cleaning Effectiveness Test Indicator
An indicator used to test the cleaning effectiveness of a washer-disinfector.
Purified water
Water that has been free of all ions, heat sources, and most microorganisms.
2.Relevant knowledge of medical sterilization supply center
01 The basic principles for demarcating work areas in the sterilization supply room are:
Logistics flow from (contaminated) to (clean), with no cross-flow or backflow.
Air flow flows from (clean) to (contaminated).
The decontamination area should maintain a temperature of 16-21°C and a relative humidity of 30-60%.
The inspection, packaging, and sterile areas should maintain a temperature of 20-23°C and a relative humidity of 30-60%.
The sterile storage area should maintain a temperature below 24°C and a relative humidity below 70%.
02 Six Standard Preventive Protective Equipment
Hats, masks, eye and face shields, gloves, protective clothing/isolation gowns, rubber boots/shoe covers, etc.
03 Hand Hygiene Indicators
4 Before and 5 After (before entering or leaving the area; after contact with contaminated/suspected contaminated items; after completing a work step and before starting a new work step; before contact with clean, disinfected, or sterilized items; after hands are contaminated/suspected contaminated; before and after putting on and removing medical gloves).
04 7-Step Handwashing Method
Inside, outside, clip, arch, large, upright, wrist.
05 Cleaning Process
(Rinse), (Wash), (Rinse), and (Final Rinse).
06 Contaminated instruments should be categorized based on their material and precision.
07 Instrument cleaning quality should be inspected visually or using a magnifying glass with a light source on each dried instrument, tool, and item. The instrument's surface and joints and teeth should be clean, free of blood, stains, scale, and other residual materials and rust, and in good working order and free of damage.

08 Packaging requirements: Scissors, vascular clamps and other axial instruments should not be completely (locked). Covered vessels should be (opened), and tubular items should be (coiled and placed) to keep the lumen unobstructed; precision instruments, sharp instruments, etc. should take (protective measures).
09 Sterilization package weight requirements: The weight of the instrument package should not exceed (7) kg, and the dressing package should not exceed (5) kg.
10 Sterilization package volume requirements: Pulsating vacuum pressure steam sterilizer should not exceed (30cmX30cmX50cm).
11 The sealing width of sealed packaging such as paper-plastic bags and paper bags should be (≥6mm), and the distance between the instrument in the package and the seal of the packaging bag should be (≥2.5cm).
12 Medical heat sealers should be checked for (accuracy of parameters) and (closure integrity) before daily use.
13 Items unloaded from the sterilizer can only be moved after the temperature drops to room temperature, and the cooling time should be (>30min).
14 Storage racks or cabinets should be at least 20 cm above the floor, 5 cm above the wall, and 50 cm above the ceiling.
15 When distributing sterile items, the first-in-first-out principle should be followed, and hands should be washed or disinfected before handling sterile items.
16 Distribution records for sterile items should be traceable and include the date of delivery, name, specification, quantity, manufacturer, batch number, sterilization date, and expiration date of single-use sterile items.
17 Biological monitoring of pressure steam sterilizers should be conducted at least weekly; biological monitoring of EO sterilizers should be conducted after each sterilization batch.
18 Recycling tools should be cleaned and disinfected after each use and kept dry for future use.
19 Packaging includes assembly, packaging, and (sealing and labeling). Instruments and dressings should not be packaged in the same room.
20 Pre-vacuum sterilizers should be empty and subjected to a B-D test before starting the sterilization run each day.
21 Sterile items should be verified for their effectiveness before distribution. Implants and implantable surgical instruments should only be distributed after passing biological monitoring.
22 Instruments used to transport sterile items should be cleaned and stored dry after use.
23 Moist Heat Disinfection Method
For diagnostic and treatment instruments, instruments, and items used directly after disinfection, the moist heat temperature should be (≥90°C, time ≥5 minutes), or (A0 value ≥3000). For further sterilization after disinfection, the moist heat temperature should be (≥90°C, time ≥1 minute, or A0 value ≥600).
24 The packaging of sterilized items should be labeled with (item name, packer), (sterilizer number, sterilization batch, sterilization date, and expiration date). The labeling should provide traceability.
25 Requirements for Textiles in Packaging Materials
They should be unbleached fabrics. The wrapping should have no seams except on the four edges and should not be repaired. Before first use, they should be (high-temperature washed, degreased, and desizing). They should be (cleaned after each use) and free of stains. Light inspection should be performed to check for damage.
26 Requirements for Disinfection and Sterilization Monitoring Materials
They should comply with relevant national standards and regulations and be used within the (expiration date).
3.Questions and Answers about the Medical Sterilization Supply Center
Q1: What are the commonly used disinfection and sterilization methods in hospitals?
Sterilization methods include: pressure steam sterilization/dry heat sterilization, ethylene oxide, hydrogen peroxide low-temperature plasma, low-temperature formaldehyde sterilization, etc.
High-level disinfection methods: Commonly used methods include the use of chlorine-containing preparations, chlorine dioxide, o-phthalaldehyde, peracetic acid, hydrogen peroxide, ozone, tincture of iodine, and other chemical disinfectants that can achieve sterilization effects, under specified conditions, at appropriate concentrations and for an effective duration.
Intermediate-level disinfection methods: Commonly used methods include the use of iodine-based disinfectants (such as iodine tinctures and chlorhexidine iodine), combinations of alcohols and chlorhexidine, combinations of alcohols and quaternary ammonium compounds, and phenols, under specified conditions, at appropriate concentrations and for an effective duration.
Low-level disinfection methods: Includes the use of disinfectants such as quaternary ammonium salts (such as benzalkonium bromide) and biguanides (chlorhexidine), under specified conditions, at appropriate concentrations and for an effective duration.
Q2: What are the basic principles and requirements for disinfection and sterilization?
Reusable diagnostic and treatment instruments, instruments, and items should be cleaned after use, then disinfected or sterilized.
Diagnostic and treatment instruments, instruments, and items contaminated with prions, gas gangrene, and pathogens of sudden, unexplained infectious diseases should be handled according to the relevant requirements for disinfection followed by cleaning, disinfection, or sterilization.
For heat- and moisture-resistant surgical instruments, pressure steam sterilization is preferred.
The environment and surfaces should generally be kept clean. However, if contaminated with a patient's blood, body fluids, or other substances, the contaminants should be removed before cleaning and disinfection.

Q3: How should disinfection and sterilization methods be selected based on the risk of infection from contaminated items?
High-risk items should be sterilized.
Moderate-risk items should be disinfected using methods that achieve a disinfection level above the intermediate level.
Low-risk items should be disinfected using low-level disinfection or cleaning. In the event of pathogenic microbial contamination, an effective disinfection method should be selected based on the type of pathogen.
Q4: What are the management requirements for disposable sterile items?
All disposable medical supplies must be used within their expiration date and may not be reused.
If the expiration date and expiration date are not clearly marked, the expiration date refers to the last day of the current month (e.g., "valid until July 2023" means valid until July 31, 2023); the expiration date refers to the last day of the previous month (e.g., "valid until July 2023" means valid until June 30, 2023).
Q5: Under what circumstances is a sterilized sterile item package considered contaminated and cannot be reused?
Before use, sterile supplies should be considered contaminated if the chemical indicator card inside the sterilized package is not completely discolored, the outer packaging is damp, the expiration date has expired, or the packaging is damaged.
Q6: How should instruments contaminated with infectious diseases be handled?
Diagnostic and treatment instruments, instruments, and items contaminated with prions, gas gangrene, or pathogens of sudden, unexplained infectious diseases should be double-sealed and labeled with the infectious disease. They should be collected and handled separately by the MSSC. Refer to the method outlined in WS/T367: disinfect first, then clean, and finally sterilize.
Q7: How should a sharp puncture wound be treated?
Immediately squeeze out the blood from the wound and rinse with running water. After rinsing, disinfect with a disinfectant (2% iodine tincture or Aner Iodine).
After handling, immediately report the injury to the department supervisor, register a sharps injury form, and report to the Infection Management Department.
The Infection Management Department and a specialist will jointly assess the injury and provide guidance on treatment.
Q8: What are the sterilization monitoring methods? What is the frequency requirement and the significance of each type of monitoring?
(1) BD test
Monitoring method and frequency: The first empty pot of each day
The actual significance of monitoring: To detect the cold air removal effect of the sterilizer
(2) Physical monitoring
Monitoring method and frequency: Each pot is carried out, focusing on monitoring the pressure, temperature and time during sterilization
The actual significance of monitoring: One of the bases for the release of sterile items
(3) Chemical monitoring
a. External chemical monitoring
Monitoring method and frequency: External chemical monitoring, each package to be sterilized
The actual significance of monitoring: One of the bases for the package to be exposed to sterilization and released
b. Internal chemical monitoring
Monitoring method and frequency: Each sterilization package is internal
The actual significance of monitoring: Basis for package use
C. Chemical batch challenge test package (chemical PCD)
Monitoring method and frequency: Each pot is carried out for non-implants
The actual significance of monitoring: An important basis for the release of sterilized items
(4) Biological monitoring
Monitoring method and frequency: Biological monitoring package, Routine monitoring is performed weekly; each batch of implants is tested.
Practical significance of monitoring: It is an important basis for implant release.
The significance of the fifth-class chemical indicator card (creeping card): It interprets the sterilization result by color shift.
The rate at which the chemical dye melts and creeps forward in the creeping card is determined by both saturated steam and the decrease in the melting point of the chemical dye.
Q9: How should a biological monitoring failure be handled?
If a biological monitoring failure occurs, the sterilizer must be discontinued, and all sterilized items that have not been used since the last successful monitoring must be recalled and reprocessed. A written report must be submitted to the relevant management department, stating the reason for the recall, and the cause must be immediately investigated.
Check that all biological indicators are within their expiration dates.
Perform a comprehensive inspection of the sterilizer, with confirmation signed by the engineering maintenance personnel. The sterilizer may only be used after three consecutive successful biological monitoring results.
Emergency handling of sterile items used clinically with this pot number:
Report to the hospital's Infectious Diseases Department and Quality Control Department → Conduct a risk assessment → Identify potentially affected patients and closely monitor clinical manifestations → Provide testing and treatment as necessary.
Analyze the incident process and steps involved, and keep detailed records.
Q10: How should chemical disinfection be monitored and recorded? (Chlorine-containing disinfectant)
Monitor the concentration after each preparation and before use, and record the start and end times of immersion disinfection and the items being immersed.
Q11: How should moist heat disinfection be monitored and recorded?
Monitor and record the temperature and time or A0 value for each disinfection.
Q12: Common measures of standard precautions
1) Hand hygiene procedures.
2) Wear gloves.
3) Proper use of mouth guards, hats, goggles, and face shields.
4) Wear protective clothing, protective shoes, waterproof aprons, and shoe covers as appropriate.
5) Appropriate protective equipment should be provided and used in different areas.
6) Handwashing and eyewash facilities should be available in decontamination areas.
7) Safety operating procedures should be in place to prevent sharp injuries.
8) Medical instruments and equipment should be cleaned and disinfected regularly.
9) Medical waste should be disposed of and managed in accordance with relevant laws and regulations.
10) The workplace, object surfaces and environment should be cleaned, disinfected and terminally disinfected at all times.

 English
English русский
русский Français
Français Español
Español bahasa Indonesia
bahasa Indonesia Deutsch
Deutsch عربى
عربى 中文简体
中文简体