The Ultimate Guide to Pressure Steam Sterilizers: Types, Uses, and Maintenance
Posted by Admin | 15 Aug
1. Introduction to Pressure Steam Sterilizers
What is a Pressure Steam Sterilizer (Autoclave)?
A Pressure Steam Sterilizer, commonly known as an autoclave, is a specialized device used to sterilize equipment, tools, and materials through high-pressure steam. The basic principle behind an autoclave is the application of heat and pressure to destroy harmful microorganisms, including bacteria, viruses, fungi, and spores. Autoclaves are widely utilized in medical, dental, laboratory, and industrial settings to ensure the safe and effective sterilization of instruments and materials that must be kept free from contamination.
Autoclaves come in various sizes, from small tabletop models to large industrial units, depending on the requirements of the environment in which they are used. Regardless of the model, they all share the same fundamental principle of using steam under pressure to achieve sterilization. This method is particularly effective because it uses moist heat, which is far more efficient at penetrating materials than dry heat.
Brief History and Evolution
The concept of using steam for sterilization dates back to the mid-19th century. The French scientist Denis Papin is often credited with developing the first pressure cooker, which laid the groundwork for autoclave technology. However, it wasn’t until 1879 that the first modern autoclave was developed by Charles Chamberland, a French biologist and collaborator of Louis Pasteur. Chamberland’s autoclave was designed specifically for sterilizing medical and laboratory equipment, and it quickly became an essential tool in hospitals and research facilities.
Over the years, autoclave technology has evolved with advances in engineering, control systems, and safety mechanisms. Early models were manual, requiring operators to carefully monitor temperature and pressure, while modern autoclaves are often equipped with sophisticated controls, automated cycles, and digital interfaces for ease of use. This evolution has significantly improved the reliability, efficiency, and versatility of autoclaves.
Importance of Sterilization in Various Fields
Sterilization plays a crucial role in a wide range of fields, from healthcare to research to manufacturing. Below are some of the primary areas where pressure steam sterilizers are indispensable:
Medical Field: In hospitals and clinics, sterilization is vital for ensuring that surgical instruments, medical devices, and waste materials are free from harmful pathogens. Contaminated equipment can lead to serious infections or even outbreaks of disease. Autoclaves provide a reliable means of maintaining hygiene standards in medical environments.
Dental Field: Just like in medicine, the dental industry relies heavily on sterilization to maintain safety and prevent the spread of infectious diseases. Dental tools, including scalers, drills, and exam instruments, are routinely sterilized using autoclaves to protect both patients and practitioners.
Laboratory: In research laboratories, autoclaves are used to sterilize a variety of materials, from glassware to culture media. Without proper sterilization, experiments and research could be contaminated by unwanted microorganisms, affecting the accuracy and safety of scientific work.
In all of these industries, the primary objective of sterilization is to destroy harmful microorganisms that could lead to infection, contamination, or inaccurate results. Without effective sterilization methods like pressure steam sterilization, the risks associated with using contaminated equipment would be far too great.
2. Principles of Steam Sterilization
How Steam Sterilization Works: Temperature, Pressure, and Time
The core mechanism behind steam sterilization lies in the interaction between high-temperature steam and the materials being sterilized. Autoclaves use a combination of temperature, pressure, and time to destroy microorganisms.
Temperature: The temperature inside an autoclave typically ranges from 121°C (250°F) to 134°C (273°F). These temperatures are necessary to effectively kill harmful bacteria, viruses, and spores. At these high temperatures, the steam penetrates the materials being sterilized, ensuring that even the most difficult-to-reach areas are exposed to the sterilizing conditions.
Pressure: Pressure plays an essential role in steam sterilization. As the steam pressure inside the autoclave increases, the boiling point of water also rises, allowing steam to reach higher temperatures. This added pressure is particularly important for ensuring that the steam can effectively penetrate through dense materials like surgical instruments or thick fabrics. The typical operating pressure in an autoclave ranges from 15 to 30 psi (pounds per square inch), depending on the specific sterilization cycle and the type of materials being sterilized.
Time: The exposure time is crucial in steam sterilization. It ensures that the sterilization conditions are maintained long enough to destroy microorganisms thoroughly. The sterilization cycle is usually measured in minutes, and the duration depends on both the temperature and the volume of material being sterilized. A typical cycle might last anywhere from 15 to 45 minutes, depending on the autoclave type and load size.
In essence, the combination of high temperature, elevated pressure, and sufficient exposure time creates an environment where microorganisms are destroyed. This process ensures that equipment and materials are not only free from bacteria but also from heat-resistant spores, which are among the hardest types of pathogens to kill.
The Science Behind Destroying Microorganisms
Steam sterilization works primarily by disrupting the cell structure of microorganisms, leading to their destruction. The high heat from the steam causes proteins and enzymes in the cells to denature, meaning they lose their natural structure and function. As a result, the cells cannot perform vital processes like replication and metabolism, leading to their death.
More specifically:
Protein Denaturation: The proteins in microbial cells, including enzymes, are sensitive to high temperatures. When exposed to steam, these proteins unfold and lose their functionality, effectively inactivating the microorganism.
Cell Membrane Disruption: The pressure and temperature of the steam can also damage the cell membrane, causing it to rupture and allowing the internal contents of the microorganism to leak out. This further ensures that the pathogen is rendered inactive.
Moisture Penetration: The moisture in the steam also helps facilitate the killing of microorganisms. Unlike dry heat, steam can penetrate materials more effectively, especially through porous surfaces, ensuring that the sterilization process reaches all parts of the object being sterilized.
Steam sterilization is also particularly effective against spores, which are dormant, heat-resistant forms of bacteria. These spores are tough to eliminate, but the conditions inside an autoclave are severe enough to break down their protective layers, rendering them harmless.
Advantages of Steam Sterilization Over Other Methods
Steam sterilization offers several distinct advantages over other sterilization techniques, making it the preferred choice in many industries. Some key benefits include:
Effectiveness Against All Microorganisms: Steam sterilization is highly effective at killing a broad range of pathogens, including bacteria, viruses, fungi, and spores. This makes it one of the most reliable sterilization methods available.
Speed and Efficiency: Autoclave sterilizer can complete sterilization cycles relatively quickly compared to other methods like dry heat or chemical sterilization. With the proper settings, an autoclave can sterilize large quantities of equipment in a short period of time, making it a highly efficient process.
Environmentally Friendly: Unlike chemical sterilization methods, which may require harmful or hazardous substances, steam sterilization uses water and heat, both of which are safe for the environment. This reduces the need for chemicals and the potential for harmful chemical residues.
Cost-Effectiveness: While autoclaves can have a significant upfront cost, they are often more cost-effective in the long term due to their durability, efficiency, and minimal ongoing maintenance requirements. The absence of chemicals also reduces recurring expenses.
Versatility: Autoclaves can sterilize a wide variety of materials, including metals, plastics, fabrics, and glass. This versatility makes them useful in multiple industries, from medical to laboratory to food processing
3. Types of Pressure Steam Sterilizers
There are various types of pressure steam sterilizers (autoclaves) designed to meet the specific needs of different industries. The choice of sterilizer depends on the materials being sterilized, the volume of sterilization, and the specific requirements of the sterilization cycle. Below, we explore the most common types of autoclaves.
Gravity Displacement Autoclaves
Gravity displacement autoclaves are the most basic type of autoclave and are commonly used in smaller settings like clinics and laboratories. In this type of autoclave, air is removed from the chamber by the force of gravity as steam is introduced. The steam then fills the chamber, displacing the air and penetrating the items being sterilized.
How It Works: The sterilization cycle begins with the air being displaced by steam, which creates the pressure needed for the sterilization process. The chamber is then heated to the required temperature, and the cycle continues until the items are exposed to steam for the necessary duration.
Advantages: These autoclaves are simple, reliable, and relatively inexpensive. They are ideal for sterilizing simple instruments that don’t require a high degree of precision or delicate handling.
Limitations: Gravity displacement autoclaves can have a hard time sterilizing porous or wrapped items because the steam may not effectively penetrate through the material. They also take longer than other types, especially when handling larger loads.
Prevacuum Autoclaves
Prevacuum autoclaves, as the name suggests, operate by first creating a vacuum inside the chamber before introducing steam. This ensures that all air is removed from the sterilizer, creating a more efficient process for sterilizing complex loads.
How It Works: A vacuum pump is used to remove air from the chamber before steam is introduced. The lack of air allows the steam to penetrate the load more effectively, ensuring that all surfaces, including porous or wrapped materials, are thoroughly sterilized.
Advantages: Prevacuum autoclaves are faster and more efficient than gravity displacement autoclaves, especially when sterilizing delicate or wrapped instruments. They offer better steam penetration, making them ideal for complex loads and high-density materials.
Limitations: These autoclaves are typically more expensive and complex to operate, requiring more maintenance than simpler models. They are also less suitable for small, basic applications.
Steam-Flush Pressure-Pulse (SFPP) Autoclaves
SFPP autoclaves use a combination of steam flushing and pressure pulses to remove air and improve the penetration of steam into difficult-to-reach areas. This type of autoclave is designed for environments where more precise control over the sterilization process is necessary.
How It Works: The cycle begins with the introduction of steam to flush out air, followed by rapid pressure pulses to further ensure that steam can reach every part of the load. The process is often repeated several times during the cycle to maximize steam penetration.
Advantages: SFPP autoclaves provide excellent sterilization results for porous and wrapped materials, offering improved consistency and reliability compared to gravity displacement or even some pre-vacuum models. They are also known for being able to handle large loads in a relatively short amount of time.
Limitations: These autoclaves can be more expensive and require a higher level of maintenance. They also tend to have more complex cycles, which may not be necessary for smaller-scale operations.
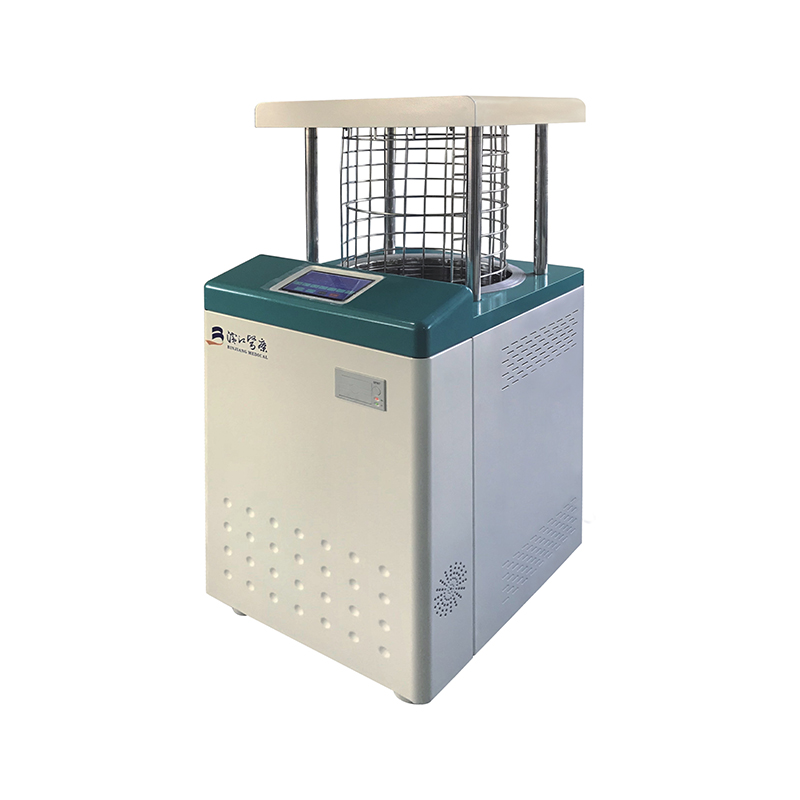
Tabletop Autoclaves
Tabletop autoclaves are compact, desktop-sized units commonly found in small medical practices, dental offices, and research labs. Despite their smaller size, they operate with the same principles as larger, industrial models, offering reliable sterilization for smaller quantities of equipment.
How It Works: Tabletop autoclaves can be gravity displacement, pre-vacuum, or SFPP types, depending on the model. They typically have smaller chambers and are designed to sterilize smaller loads quickly and efficiently.
Advantages: Their compact size makes them perfect for smaller settings where space is limited. Tabletop autoclaves are also relatively easy to use and maintain, making them ideal for smaller medical or dental offices.
Limitations: Due to their size, these autoclaves typically have a lower capacity compared to larger models, meaning they may not be suitable for high-volume operations.
Large Capacity Autoclaves
Large capacity steam autoclaves are industrial-sized machines designed to handle larger loads of equipment and materials. These autoclaves are typically used in hospitals, research facilities, pharmaceutical industries, and manufacturing environments where bulk sterilization is required.
How It Works: These autoclaves often use pre-vacuum or SFPP technology to ensure efficient sterilization. They are equipped with larger chambers and more powerful steam and vacuum systems to handle high volumes of materials.
Advantages: Large capacity autoclaves are ideal for high-volume sterilization, offering the ability to process large batches of materials quickly and effectively. They are often equipped with sophisticated monitoring and control systems, ensuring precise sterilization cycles.
Limitations: Due to their size, these autoclaves require significant space and often come with higher upfront costs. They may also require specialized installation and maintenance.
Choosing the Right Type for Your Needs
Selecting the right type of pressure steam sterilizer depends on several factors, including:
Type of materials to be sterilized: Consider whether you’ll be sterilizing wrapped instruments, porous materials, liquids, or large batches. Some autoclaves, like pre-vacuum and SFPP models, are better suited for complex loads.
Volume of sterilization: Smaller clinics or laboratories may benefit from tabletop models, while larger hospitals and industries may need large capacity autoclaves to handle higher volumes.
Budget and space constraints: Tabletop autoclaves are more affordable and space-efficient, while larger models offer more capabilities but come with a higher cost and space requirement.
4. Applications of Pressure Steam Sterilizers
Pressure steam sterilizers (autoclaves) have widespread applications across various industries, each with its unique requirements for sterilization. Below, we’ll explore how autoclaves are used in different sectors and why they are indispensable in maintaining safety, quality, and hygiene.
Medical Field: Surgical Instruments, Medical Waste
In the medical field, autoclaves are essential for ensuring that surgical instruments, diagnostic tools, and other medical equipment are completely sterile before use. Infection control is a top priority in healthcare, and autoclaves help eliminate the risk of cross-contamination between patients.
Surgical Instruments: Autoclaves sterilize items like scalpels, forceps, scissors, and other reusable surgical tools. Given the high risk of infection associated with surgical procedures, autoclaving ensures that all instruments are free from harmful microorganisms.
Medical Waste: Autoclaves are also used to sterilize medical waste, such as contaminated dressings, syringes, and other disposable items. This is particularly important in hospitals and clinics, where large volumes of potentially infectious waste are generated daily.
Sterilization through autoclaving helps prevent the spread of infections and maintains the safety of both patients and healthcare workers.
Dental Field: Dental Tools and Equipment
Dental professionals rely heavily on autoclaves to sterilize their tools and equipment between patient visits. The close proximity to patients during dental procedures makes it vital to maintain the highest hygiene standards.
Dental Tools: Instruments like drills, scalers, tweezers, and mouth mirrors must be sterilized after each use to prevent the spread of bacteria, viruses, or fungi. Autoclaves ensure that dental tools are disinfected thoroughly, maintaining a safe environment for both patients and practitioners.
Other Dental Equipment: Besides tools, autoclaves are also used to sterilize other equipment, such as impressions, prostheses, and orthodontic devices. Ensuring these items are free of pathogens is critical in avoiding cross-contamination between patients.
Sterilization in the dental field also prevents the spread of bloodborne diseases like hepatitis and HIV, which can be transmitted through contaminated equipment.
Laboratory Field: Sterilizing Media, Glassware
In laboratories, autoclaves are indispensable for sterilizing a variety of items, ranging from glassware to biological media used in experiments and research.
Sterilizing Glassware: Glass items such as petri dishes, test tubes, and flasks are frequently sterilized in autoclaves before being used in experiments. This prevents contamination from microorganisms that could compromise research findings.
Sterilizing Media: In microbiology labs, culture media—such as agar plates and broth—are autoclaved to eliminate any microorganisms before being inoculated with the intended sample. This is crucial for ensuring the accuracy of microbial studies and experiments.
Sterilizing Equipment: Autoclaves are also used to sterilize various lab instruments, such as pipettes, forceps, and petri dishes, all of which need to be free of contaminants to ensure valid and reproducible results.
In the laboratory setting, autoclaves are crucial for ensuring that experiments and research are conducted under sterile conditions, which is especially vital in fields like microbiology, genetics, and molecular biology.
Pharmaceutical Industry: Sterilizing Solutions, Equipment
The pharmaceutical industry relies heavily on sterilization to ensure that the drugs, solutions, and equipment used in production are free of microbial contamination. This is crucial in the manufacturing of medications and vaccines, where even the smallest contamination can lead to disastrous results.
Sterilizing Pharmaceutical Equipment: Autoclaves are used to sterilize pharmaceutical manufacturing equipment such as mixing tanks, storage containers, and tubing. Ensuring that these items are free of microbial life is essential for maintaining the quality and safety of the final products.
Sterilizing Solutions: Some pharmaceutical solutions, especially injectable medications, require sterilization before being packaged for sale. Autoclaves are used to sterilize these products at high temperatures to ensure they are free of harmful microorganisms.
In addition, autoclaves are used to sterilize other critical items in the production process, such as vials, stoppers, and syringes, all of which must be free of contaminants before being filled with pharmaceutical solutions.
Other Industries: Food, Veterinary, Tattoo
Pressure steam sterilizers are also used in several other industries where sterilization is required for both safety and quality control.
Food Industry: In the food industry, autoclaves are used for canning and preserving food products. The process, known as retort sterilization, involves sealing food in containers and then exposing it to high-pressure steam to kill bacteria and extend shelf life. This process is commonly used for items like canned vegetables, meats, and soups.
Veterinary: In veterinary practices, autoclaves are used to sterilize surgical tools, medical waste, and other equipment. Just like in human medicine, preventing the spread of diseases in animals is a priority, and autoclaves help ensure that tools and instruments are sterilized and safe for use in procedures.
Tattoo Industry: In the tattoo industry, sterilizing needles, ink caps, and other tools is vital for preventing infections and ensuring safe practices. Autoclaves are commonly used in tattoo parlors to sterilize the equipment between uses.
5. The Sterilization Process: A Step-by-Step Guide
Sterilizing items using a pressure steam sterilizer involves a series of well-defined steps to ensure that every item is thoroughly sterilized and safe for use. Here's a breakdown of the process from start to finish:
Preparation of Materials
Before loading the items into the autoclave, preparation is key to ensure that the sterilization process goes smoothly and effectively.
Cleaning: All items must be thoroughly cleaned to remove visible dirt, debris, or biological material. Any residue left on instruments can protect microorganisms, making sterilization less effective. It's important to clean tools and equipment before autoclaving them, either manually or in an ultrasonic cleaner, depending on the items being sterilized.
Wrapping: For many instruments, especially surgical or dental tools, wrapping is essential. The wrapping—usually in sterilization wraps or pouches—helps keep the instruments sterile after they leave the autoclave. It also allows for easier handling once the cycle is complete. The wrapping ensures that the tools remain protected from re-contamination after sterilization.
Proper Loading: Proper loading is critical to ensure steam can circulate freely and reach all surfaces of the items being sterilized. Items should be placed in the autoclave in such a way that they don’t touch the chamber walls or each other. Overcrowding the autoclave can lead to incomplete sterilization.
Loading the Autoclave
Once materials are cleaned and wrapped, they are ready to be placed inside the autoclave.
Chamber Capacity: Be mindful not to exceed the recommended load capacity of the autoclave. Overloading can prevent steam from circulating properly, leading to inefficient sterilization.
Load Distribution: Items should be placed in a way that allows proper steam flow and air removal. For example, heavier items should be placed on the bottom, and instruments should be positioned to allow steam to reach all surfaces. Special trays or baskets may be used to hold smaller items or instruments.
Steam Penetration: Items that are wrapped or porous may need additional attention to ensure steam reaches all surfaces. For example, for wrapped instruments, the wrapping must not block steam access to the items inside. Prevacuum and SFPP autoclaves are particularly effective in this regard, as they help remove air and allow steam to penetrate more thoroughly.
Selecting the Appropriate Cycle
Autoclaves come with different sterilization cycles that are tailored to specific materials and requirements. Selecting the right cycle ensures that sterilization occurs at the appropriate temperature, pressure, and time.
Cycle Parameters: The parameters will depend on the type of autoclave you are using, as well as the items being sterilized. Common cycles include:
Standard cycle: Often set at 121°C (250°F) for around 15-20 minutes at 15-20 psi pressure, ideal for most general sterilization needs.
High-temperature cycle: Sometimes used for heat-resistant materials, typically at 134°C (273°F) for a shorter cycle, around 3-5 minutes.
Liquid cycle: For sterilizing liquids like culture media or pharmaceuticals, a gentle cycle is used to avoid boiling or contamination of the liquid.
Cycle Monitoring: Most modern autoclaves come with built-in monitoring systems that ensure the cycle runs correctly. These systems monitor temperature, pressure, and time to ensure that the desired sterilization conditions are met. Operators should always verify that the cycle parameters are set according to the manufacturer's guidelines.
Running the Sterilization Cycle
Once the cycle has been selected and the autoclave is loaded, it’s time to begin the sterilization process.
Temperature and Pressure Build-Up: The autoclave first raises the pressure and temperature to the desired level. During this phase, air is either displaced or removed (in the case of pre-vacuum and SFPP autoclaves), allowing steam to fill the chamber. The temperature continues to rise until it reaches the set point, typically around 121°C (250°F) or 134°C (273°F).
Exposure Time: After the target temperature and pressure have been reached, the autoclave will maintain those conditions for a specified period, ensuring complete sterilization. The exposure time varies depending on the type of materials and autoclave cycle chosen.
Cycle Monitoring: Many autoclaves are equipped with digital systems that track the sterilization cycle’s progress and will alert operators if any problems occur during the cycle. For older manual models, operators need to monitor the process closely to ensure everything runs smoothly.
Unloading and Storing Sterilized Items
Once the sterilization cycle is complete, the autoclave will begin the cooling phase, during which pressure and temperature return to normal.
Cool Down: Before opening the autoclave, it’s essential to allow it to cool down to a safe temperature. Opening the door too soon can result in burns or contamination as air rushes into the chamber. Additionally, some autoclaves have drying cycles that help remove excess moisture from items after sterilization.
Safe Unloading: When it’s safe to open the door, carefully remove the sterilized items, being cautious not to touch the inside of the autoclave chamber or the sterilized items. Using heat-resistant gloves or tongs is advised.
Storage: After sterilization, items should be stored in a sterile environment. For wrapped instruments, the wrapping helps maintain sterility, but for unwrapped items, sterile storage containers or cabinets should be used to prevent contamination.
6. Validation and Monitoring
Ensuring that the sterilization process is consistently effective is critical for maintaining safety standards. This is where validation and monitoring come into play. Both are essential for confirming that the autoclave is working properly and that sterilization has been successfully achieved.
Importance of Validation
Validation refers to the process of confirming that an autoclave consistently performs its sterilization cycle according to its intended parameters (temperature, pressure, time). It is vital for several reasons:
Preventing Contamination: If an autoclave fails to reach the required sterilization conditions, the items inside may not be properly sterilized, leading to potential contamination risks.
Compliance with Standards: Validation ensures compliance with industry regulations and standards, such as those set by the FDA, CDC, and ISO. Regular validation is necessary for meeting these requirements, particularly in medical and pharmaceutical industries.
Process Control: Continuous validation helps monitor the overall sterilization process, ensuring that there are no deviations from set parameters. This is critical for ensuring the long-term reliability of sterilization procedures.
Types of Sterilization Indicators: Biological, Chemical, and Physical
There are three main types of indicators used to validate and monitor the sterilization process. Each type provides different levels of assurance that the items have been sterilized correctly.
Biological Indicators (BIs)
What They Are: Biological indicators are small vials or test strips containing highly resistant bacterial spores, such as Geobacillus stearothermophilus, which are known to withstand autoclave conditions. These spores are used to test whether the autoclave was able to kill even the most resistant microorganisms.
How They Work: After sterilization, the biological indicator is cultured to see if any spores have survived. If no growth occurs, it confirms that the autoclave has successfully killed all the microorganisms, including spores. If growth is detected, the cycle did not achieve the necessary conditions for sterilization, and corrective actions should be taken.
Advantages: Biological indicators provide the highest level of assurance that sterilization has occurred because they directly measure the lethality of the autoclave's conditions.
Chemical Indicators (CIs)
What They Are: Chemical indicators are substances that change color or form when exposed to certain conditions (e.g., temperature, pressure, and time). They are typically used as quick, visual confirmation that the sterilization cycle was completed.
How They Work: CIs are placed on the items being sterilized or inside the autoclave. After the sterilization cycle, the indicators are examined. If they show a color change, it suggests that the items inside were exposed to the required conditions for sterilization.
Advantages: Chemical indicators are easy to use and provide quick feedback. However, they do not guarantee that sterilization was successful; they only confirm that the correct conditions (temperature, pressure, etc.) were reached during the cycle.
Physical Indicators
What They Are: Physical indicators are the built-in gauges and monitoring systems that track parameters like temperature, pressure, and cycle time during the sterilization process. These are often displayed on the autoclave's control panel.
How They Work: These indicators allow operators to monitor the real-time status of the autoclave cycle. If the temperature and pressure levels fall within the designated range and the cycle time is appropriate, it provides assurance that the sterilization conditions were met.
Advantages: Physical indicators are essential for confirming that the autoclave is operating as intended. However, like chemical indicators, they don’t directly measure whether the microbial life was effectively destroyed—they only show the conditions that were reached during the cycle.
Regular Testing and Monitoring Procedures
Regular testing and monitoring are necessary to maintain the efficacy of autoclaves over time. Routine checks help ensure that the equipment continues to meet sterilization standards. Key procedures include:
Daily Monitoring: On a daily basis, operators should monitor the autoclave’s performance by reviewing its physical indicators (temperature, pressure, and cycle time). This will ensure that the machine is operating within the necessary parameters.
Biological Testing: Biological indicators should be used at regular intervals (e.g., weekly) to validate the autoclave’s performance. The frequency of this testing will depend on the facility's standards and regulatory requirements.
Chemical Indicator Testing: Chemical indicators can be used for more frequent checks, either with each sterilization cycle or after a set number of cycles. These indicators are particularly useful for confirming that sterilization conditions were met, but should not replace biological testing for comprehensive validation.
Maintenance and Calibration: Autoclaves should undergo regular calibration to ensure their components (e.g., sensors, temperature probes) are functioning correctly. Calibration should be performed as per the manufacturer’s guidelines, often on a yearly basis or whenever there is a malfunction.
Record Keeping: Detailed records of all validation and monitoring activities should be maintained. This includes the results of biological, chemical, and physical tests, along with maintenance and repair logs. Keeping thorough documentation is essential for quality control, as well as for compliance with regulatory bodies.
6. Validation and Monitoring
Ensuring that the sterilization process is consistently effective is critical for maintaining safety standards. This is where validation and monitoring come into play. Both are essential for confirming that the autoclave is working properly and that sterilization has been successfully achieved.
Importance of Validation
Validation refers to the process of confirming that an autoclave consistently performs its sterilization cycle according to its intended parameters (temperature, pressure, time). It is vital for several reasons:
Preventing Contamination: If an autoclave fails to reach the required sterilization conditions, the items inside may not be properly sterilized, leading to potential contamination risks.
Compliance with Standards: Validation ensures compliance with industry regulations and standards, such as those set by the FDA, CDC, and ISO. Regular validation is necessary for meeting these requirements, particularly in medical and pharmaceutical industries.
Process Control: Continuous validation helps monitor the overall sterilization process, ensuring that there are no deviations from set parameters. This is critical for ensuring the long-term reliability of sterilization procedures.
Types of Sterilization Indicators: Biological, Chemical, and Physical
There are three main types of indicators used to validate and monitor the sterilization process. Each type provides different levels of assurance that the items have been sterilized correctly.
Biological Indicators (BIs)
What They Are: Biological indicators are small vials or test strips containing highly resistant bacterial spores, such as Geobacillus stearothermophilus, which are known to withstand autoclave conditions. These spores are used to test whether the autoclave was able to kill even the most resistant microorganisms.
How They Work: After sterilization, the biological indicator is cultured to see if any spores have survived. If no growth occurs, it confirms that the autoclave has successfully killed all the microorganisms, including spores. If growth is detected, the cycle did not achieve the necessary conditions for sterilization, and corrective actions should be taken.
Advantages: Biological indicators provide the highest level of assurance that sterilization has occurred because they directly measure the lethality of the autoclave's conditions.
Chemical Indicators (CIs)
What They Are: Chemical indicators are substances that change color or form when exposed to certain conditions (e.g., temperature, pressure, and time). They are typically used as quick, visual confirmation that the sterilization cycle was completed.
How They Work: CIs are placed on the items being sterilized or inside the autoclave. After the sterilization cycle, the indicators are examined. If they show a color change, it suggests that the items inside were exposed to the required conditions for sterilization.
Advantages: Chemical indicators are easy to use and provide quick feedback. However, they do not guarantee that sterilization was successful; they only confirm that the correct conditions (temperature, pressure, etc.) were reached during the cycle.
Physical Indicators
What They Are: Physical indicators are the built-in gauges and monitoring systems that track parameters like temperature, pressure, and cycle time during the sterilization process. These are often displayed on the autoclave's control panel.
How They Work: These indicators allow operators to monitor the real-time status of the autoclave cycle. If the temperature and pressure levels fall within the designated range and the cycle time is appropriate, it provides assurance that the sterilization conditions were met.
Advantages: Physical indicators are essential for confirming that the autoclave is operating as intended. However, like chemical indicators, they don’t directly measure whether the microbial life was effectively destroyed—they only show the conditions that were reached during the cycle.
Regular Testing and Monitoring Procedures
Regular testing and monitoring are necessary to maintain the efficacy of autoclaves over time. Routine checks help ensure that the equipment continues to meet sterilization standards. Key procedures include:
Daily Monitoring: On a daily basis, operators should monitor the autoclave’s performance by reviewing its physical indicators (temperature, pressure, and cycle time). This will ensure that the machine is operating within the necessary parameters.
Biological Testing: Biological indicators should be used at regular intervals (e.g., weekly) to validate the autoclave’s performance. The frequency of this testing will depend on the facility's standards and regulatory requirements.
Chemical Indicator Testing: Chemical indicators can be used for more frequent checks, either with each sterilization cycle or after a set number of cycles. These indicators are particularly useful for confirming that sterilization conditions were met, but should not replace biological testing for comprehensive validation.
Maintenance and Calibration: Autoclaves should undergo regular calibration to ensure their components (e.g., sensors, temperature probes) are functioning correctly. Calibration should be performed as per the manufacturer’s guidelines, often on a yearly basis or whenever there is a malfunction.
Record Keeping: Detailed records of all validation and monitoring activities should be maintained. This includes the results of biological, chemical, and physical tests, along with maintenance and repair logs. Keeping thorough documentation is essential for quality control, as well as for compliance with regulatory bodies.
6. Validation and Monitoring
Ensuring that the sterilization process is consistently effective is critical for maintaining safety standards. This is where validation and monitoring come into play. Both are essential for confirming that the autoclave is working properly and that sterilization has been successfully achieved.
Importance of Validation
Validation refers to the process of confirming that an autoclave consistently performs its sterilization cycle according to its intended parameters (temperature, pressure, time). It is vital for several reasons:
Preventing Contamination: If an autoclave fails to reach the required sterilization conditions, the items inside may not be properly sterilized, leading to potential contamination risks.
Compliance with Standards: Validation ensures compliance with industry regulations and standards, such as those set by the FDA, CDC, and ISO. Regular validation is necessary for meeting these requirements, particularly in medical and pharmaceutical industries.
Process Control: Continuous validation helps monitor the overall sterilization process, ensuring that there are no deviations from set parameters. This is critical for ensuring the long-term reliability of sterilization procedures.
Types of Sterilization Indicators: Biological, Chemical, and Physical
There are three main types of indicators used to validate and monitor the sterilization process. Each type provides different levels of assurance that the items have been sterilized correctly.
Biological Indicators (BIs)
What They Are: Biological indicators are small vials or test strips containing highly resistant bacterial spores, such as Geobacillus stearothermophilus, which are known to withstand autoclave conditions. These spores are used to test whether the autoclave was able to kill even the most resistant microorganisms.
How They Work: After sterilization, the biological indicator is cultured to see if any spores have survived. If no growth occurs, it confirms that the autoclave has successfully killed all the microorganisms, including spores. If growth is detected, the cycle did not achieve the necessary conditions for sterilization, and corrective actions should be taken.
Advantages: Biological indicators provide the highest level of assurance that sterilization has occurred because they directly measure the lethality of the autoclave's conditions.
Chemical Indicators (CIs)
What They Are: Chemical indicators are substances that change color or form when exposed to certain conditions (e.g., temperature, pressure, and time). They are typically used as quick, visual confirmation that the sterilization cycle was completed.
How They Work: CIs are placed on the items being sterilized or inside the autoclave. After the sterilization cycle, the indicators are examined. If they show a color change, it suggests that the items inside were exposed to the required conditions for sterilization.
Advantages: Chemical indicators are easy to use and provide quick feedback. However, they do not guarantee that sterilization was successful; they only confirm that the correct conditions (temperature, pressure, etc.) were reached during the cycle.
Physical Indicators
What They Are: Physical indicators are the built-in gauges and monitoring systems that track parameters like temperature, pressure, and cycle time during the sterilization process. These are often displayed on the autoclave's control panel.
How They Work: These indicators allow operators to monitor the real-time status of the autoclave cycle. If the temperature and pressure levels fall within the designated range and the cycle time is appropriate, it provides assurance that the sterilization conditions were met.
Advantages: Physical indicators are essential for confirming that the autoclave is operating as intended. However, like chemical indicators, they don’t directly measure whether the microbial life was effectively destroyed—they only show the conditions that were reached during the cycle.
Regular Testing and Monitoring Procedures
Regular testing and monitoring are necessary to maintain the efficacy of autoclaves over time. Routine checks help ensure that the equipment continues to meet sterilization standards. Key procedures include:
Daily Monitoring: On a daily basis, operators should monitor the autoclave’s performance by reviewing its physical indicators (temperature, pressure, and cycle time). This will ensure that the machine is operating within the necessary parameters.
Biological Testing: Biological indicators should be used at regular intervals (e.g., weekly) to validate the autoclave’s performance. The frequency of this testing will depend on the facility's standards and regulatory requirements.
Chemical Indicator Testing: Chemical indicators can be used for more frequent checks, either with each sterilization cycle or after a set number of cycles. These indicators are particularly useful for confirming that sterilization conditions were met, but should not replace biological testing for comprehensive validation.
Maintenance and Calibration: Autoclaves should undergo regular calibration to ensure their components (e.g., sensors, temperature probes) are functioning correctly. Calibration should be performed as per the manufacturer’s guidelines, often on a yearly basis or whenever there is a malfunction.
Record Keeping: Detailed records of all validation and monitoring activities should be maintained. This includes the results of biological, chemical, and physical tests, along with maintenance and repair logs. Keeping thorough documentation is essential for quality control, as well as for compliance with regulatory bodies.
9. Regulatory Standards and Guidelines
Autoclave use, particularly in medical, dental, laboratory, and industrial settings, is subject to stringent regulatory standards. Compliance with these standards ensures that sterilization processes are carried out safely and effectively, and that the autoclave meets industry requirements for performance and safety. Here are some of the key regulations and guidelines you should be aware of.
FDA Regulations
The U.S. Food and Drug Administration (FDA) is responsible for regulating medical devices, including autoclaves, that are used in healthcare settings. FDA regulations ensure that autoclaves meet the required standards for safety, effectiveness, and quality.
Class II Medical Devices: Most autoclaves used in medical settings are classified as Class II medical devices, meaning they are subject to FDA oversight but can be marketed once certain criteria are met. Manufacturers must provide evidence that their devices are safe and effective for sterilization purposes through testing and documentation.
510(k) Premarket Notification: Before selling an autoclave in the U.S., manufacturers must submit a 510(k) premarket notification to the FDA, demonstrating that the device is substantially equivalent to another legally marketed device.
Performance Standards: The FDA requires that autoclaves used for sterilization be tested for performance, ensuring they meet specific parameters such as temperature, pressure, and time for effective sterilization.
FDA Inspections: Regular inspections and audits are performed to ensure compliance with good manufacturing practices (GMP), including the proper validation of sterilization cycles and maintenance of equipment.
CDC Guidelines
The Centers for Disease Control and Prevention (CDC) provides comprehensive guidelines for infection control and sterilization practices in healthcare settings, including the use of autoclaves.
Sterilization and Disinfection Guidelines: The CDC’s Guideline for Disinfection and Sterilization in Healthcare Facilities outlines the standards for sterilizing medical and dental instruments using pressure steam sterilizers. These guidelines focus on ensuring that sterilization cycles are adequately validated and that autoclaves are maintained and operated correctly.
Infection Prevention: CDC guidelines emphasize the importance of sterilizing instruments to prevent healthcare-associated infections (HAIs). Autoclaves must meet specific standards to ensure that all microbial life is eliminated from surgical instruments, dental tools, and other medical equipment.
Monitoring and Testing: The CDC recommends regular monitoring of autoclave performance using biological indicators (BIs), chemical indicators (CIs), and physical indicators. They also advise routine testing to confirm that the autoclave is functioning within validated parameters.
ISO Standards
The International Organization for Standardization (ISO) has developed a number of standards related to sterilization and autoclaves. These standards ensure that autoclaves are safe, effective, and reliable for use in various industries.
ISO 17665-1: This standard outlines the requirements for steam sterilization of healthcare products. It provides guidance on the development, validation, and routine control of the sterilization process. This includes specifying parameters like temperature, pressure, and exposure time for different types of autoclaves.
ISO 13485: This standard is specific to quality management systems for medical devices, including autoclaves. It ensures that the manufacturing processes meet regulatory requirements and that devices consistently perform according to specification. Compliance with ISO 13485 is necessary for manufacturers wishing to market autoclaves for medical use.
ISO 9001: While not specific to autoclaves, ISO 9001 is a widely recognized standard for quality management systems that ensures manufacturers produce high-quality, reliable products. Autoclave manufacturers adhering to this standard demonstrate their commitment to producing reliable equipment.
Other Relevant Standards
In addition to FDA, CDC, and ISO regulations, there are various national and international standards that may apply depending on the region and application of the autoclave. Some of these include:
EN 285: This European standard defines the requirements for steam sterilizers used in healthcare settings. It focuses on the technical specifications, performance, and validation of autoclaves.
ANSI/AAMI ST79: Published by the Association for the Advancement of Medical Instrumentation (AAMI), this standard provides detailed guidelines on steam sterilization in healthcare settings. It includes recommendations for operation, testing, maintenance, and validation of autoclaves.
TGA (Therapeutic Goods Administration): In countries like Australia, the TGA regulates medical devices, including autoclaves, to ensure they meet safety and performance standards for use in healthcare facilities.
10. Recent Innovations in Pressure Steam Sterilizer Technology
Technology in the field of pressure steam sterilization has evolved significantly over the years. With the need for more efficient, reliable, and cost-effective sterilization solutions, various innovations have emerged. These advancements are not only improving sterilization effectiveness but also enhancing safety, reducing energy consumption, and making autoclaves smarter and easier to use.
1. Advanced Control Systems
One of the most significant innovations in autoclave technology is the development of advanced control systems. These systems offer enhanced automation, precision, and user-friendly interfaces.
Microprocessor-Based Controls: Modern autoclaves are increasingly equipped with microprocessor-based control systems. These systems allow for more precise control over temperature, pressure, and sterilization cycle times. They also offer easy-to-use touchscreens for quick adjustments and programming.
Multi-Stage Sterilization Cycles: Newer autoclaves come with the ability to run multi-stage cycles tailored for specific types of loads (e.g., textiles, liquids, or instruments). This feature improves the flexibility of the autoclave, allowing operators to sterilize a variety of materials more efficiently.
Smart Features: Advanced autoclaves can now connect to networks via Wi-Fi or Ethernet, allowing for remote monitoring and control. Operators can track the sterilization process in real time and receive notifications if any parameters fall out of specification. This helps reduce human error and improves overall safety.
Data Logging and Traceability: Many modern autoclaves now include data logging functionality, which records detailed data throughout the sterilization cycle. This data is often stored in a digital format and can be used for validation, regulatory compliance, and audit trails. Some systems even generate certificates of sterilization automatically after a cycle.
2. Energy Efficiency Improvements
Energy efficiency is an ongoing concern in many industries, and autoclaves are no exception. As concerns about sustainability and operational costs grow, manufacturers are integrating energy-saving technologies into pressure steam sterilizers.
Heat Recovery Systems: Newer autoclaves incorporate heat recovery systems that capture the heat from exhaust steam and use it to pre-heat incoming water. This reduces the energy needed to reach the necessary sterilization temperature, improving overall efficiency.
Faster Cycle Times: Advances in both the design and control systems of autoclaves have led to faster sterilization cycles, which reduce energy consumption per load. Autoclaves are now designed to achieve sterilization conditions more quickly, shortening the overall cycle time without compromising the effectiveness of sterilization.
Low-Volume, High-Efficiency Models: Smaller, tabletop autoclaves are also becoming more energy-efficient. These models are specifically designed for low-volume sterilization but incorporate technologies such as vacuum pre-evacuation and efficient heating elements to reduce energy usage.
3. Connectivity and Data Logging
The trend towards smart autoclaves with connectivity and data logging capabilities is transforming how sterilization operations are monitored and documented.
Remote Monitoring: Many modern autoclaves can be linked to a central system that allows for real-time monitoring from remote locations. This is especially useful in larger facilities where multiple autoclaves are in operation, as it enables facility managers to track all machines simultaneously and intervene if any issues arise.
Data Logging and Reporting: Data logging has become a crucial feature in modern autoclaves. The system automatically records parameters such as temperature, pressure, cycle time, and load type for each sterilization run. This data is essential for traceability and quality control, allowing operators to verify that the sterilization process met the necessary standards.
Cloud Integration: Some manufacturers now offer cloud-based platforms where data from autoclaves can be stored securely and accessed anywhere. This is particularly beneficial for compliance, allowing easy access to sterilization records for audits or inspections without the need to manually track physical logs.
4. Improved Safety Features
Recent innovations in autoclave technology also emphasize enhanced safety, reducing the risk of accidents or malfunctions that could endanger operators or the environment.
Automatic Door Locking Mechanism: Many autoclaves now feature automatic door-locking mechanisms that prevent the door from being opened while the autoclave is still pressurized. This safety feature eliminates the risk of steam burns or sudden pressure release during the cycle.
Pressure Relief Valves and Safety Alarms: Newer autoclaves are equipped with automated pressure relief valves and safety alarms that trigger if there’s a malfunction in the pressure or temperature system. These safety systems are designed to automatically release pressure in the event of a malfunction, preventing dangerous situations from occurring.
Visual and Audio Alerts: Modern autoclaves come with visual and audio alerts to notify operators if there is an issue with the sterilization cycle. These alerts can indicate problems such as temperature deviations, cycle time issues, or door seal failures.
5. Environmental Sustainability
Sustainability is a growing concern in all industries, and autoclave manufacturers are responding by focusing on reducing the environmental impact of sterilization.
Water Conservation: Many new autoclaves incorporate features designed to minimize water usage, such as closed-loop water systems. These systems recycle water used during the sterilization cycle, which can significantly reduce water consumption.
Eco-Friendly Materials: Manufacturers are also adopting more eco-friendly materials for autoclave construction, such as recyclable metals and plastics, as part of their commitment to reducing environmental footprints.
Low-Emissions Systems: Modern autoclaves are designed to minimize emissions from the sterilization process, which can be especially important in industries where strict environmental regulations apply.
11. Choosing the Right Pressure Steam Sterilizer
Selecting the appropriate pressure steam sterilizer (autoclave) for your needs is crucial to ensuring that your sterilization processes are both effective and efficient. With various types and models available, understanding your specific requirements can help you choose the right machine. Factors such as capacity, cycle time, features, and budget all play a role in making the best decision.
1. Factors to Consider: Capacity, Cycle Time, Features, Budget
Choosing the right autoclave begins with evaluating your specific needs. Here are the main factors to consider:
Capacity:
The capacity of an autoclave determines how much material it can sterilize in one cycle. If you are running a small clinic or laboratory, a tabletop or small-capacity autoclave may be sufficient. For larger facilities like hospitals or industrial operations, you may need a larger capacity model to handle higher volumes of materials. It's important to consider the volume of items you plan to sterilize on a daily basis.
Cycle Time:
Autoclaves vary in how long they take to complete a sterilization cycle. For high-throughput environments, you’ll want a model with faster cycle times to maximize efficiency. Keep in mind, however, that shorter cycles should not compromise the effectiveness of sterilization. Prevacuum autoclaves and SFPP autoclaves tend to offer faster cycles compared to gravity displacement types, so this is a key factor if speed is critical for your operations.
Type of Load:
Different types of loads (e.g., liquids, solids, porous materials) may require different sterilization methods. Some autoclaves are specifically designed for certain load types:
Gravity displacement autoclaves are generally used for solid items like surgical tools.
Prevacuum and SFPP autoclaves are ideal for porous materials and instruments that require a vacuum phase before sterilization to ensure steam penetration.
Features:
Modern autoclaves come with a wide range of features that can enhance convenience, safety, and efficiency. Look for features such as:
Automatic cycle control and programmable settings to customize sterilization cycles based on your needs.
Built-in data logging and connectivity options for real-time monitoring and reporting.
Vacuum drying cycles for effective drying of porous materials or instruments after sterilization.
Automatic door locking mechanisms for safety, ensuring the door cannot be opened while the chamber is pressurized.
Budget:
Autoclaves are available at a wide range of price points, depending on the features, size, and complexity of the model. While larger and more advanced autoclaves offer more features, they also come with a higher price tag. It's important to balance your budget with your facility's sterilization requirements. Keep in mind that the initial cost may also include installation, maintenance, and operational costs.
2. Types of Autoclaves Based on Application
Autoclaves come in different models, each suited to specific applications. Here’s a quick guide to help you understand the different types and their best uses:
Gravity Displacement Autoclaves:
These are the most basic and traditional types of autoclaves. Gravity displacement autoclaves use gravity to remove air from the chamber, allowing steam to penetrate the items being sterilized. They are well-suited for solid materials and non-porous items like surgical instruments.
Best For: Routine sterilization of instruments, glassware, and other non-porous items.
Prevacuum Autoclaves:
Prevacuum autoclaves use a vacuum pump to remove air from the chamber before steam is introduced. This ensures that the steam can penetrate more thoroughly, making them ideal for porous materials or items with complex geometries. These models typically offer faster cycle times compared to gravity displacement autoclaves.
Best For: Sterilizing porous materials, textiles, and complex instruments that require deep steam penetration.
Steam-Flush Pressure-Pulse (SFPP) Autoclaves:
SFPP autoclaves operate by creating a series of pressure pulses combined with steam flushing, ensuring thorough sterilization, especially for difficult-to-sterilize items like wrapped instruments and porous materials. These machines are generally faster and more effective than gravity displacement models.
Best For: Medical and dental tools, sterilizing wrapped instruments, and porous loads.
Tabletop Autoclaves:
These are compact models that are ideal for small labs, dental offices, and clinics. Tabletop autoclaves are generally lower capacity but are highly effective for small-scale sterilization tasks. They are also easier to maintain and operate.
Best For: Small clinics, dental practices, and laboratories with limited sterilization needs.
Large Capacity Autoclaves:
Larger models are used in hospitals, research facilities, and industrial applications where there is a need to sterilize large volumes of material. These autoclaves often have multiple chambers and can handle large, heavy loads.
Best For: Hospitals, research institutions, and industrial applications with high-volume sterilization needs.
3. Top Brands and Models
When choosing an autoclave, it’s also important to consider the brand and model. Some brands are known for their reliability, quality, and customer support. Here are some of the top brands in the autoclave industry:
Tuttnauer: A well-known brand that offers a variety of models, including gravity displacement and pre-vacuum autoclaves, known for their reliability and ease of use.
Getinge: A leading provider of sterilization equipment, Getinge offers high-quality autoclaves that are commonly used in healthcare and research facilities.
Steris: Known for its advanced autoclaves, Steris provides machines that incorporate modern technologies like data logging and automatic cycle control.
Pelton & Crane: Specializes in dental autoclaves, offering compact models that provide efficient and reliable sterilization for dental instruments.
Amsco: Known for its high-performance autoclaves, Amsco’s models are designed for large healthcare facilities and laboratories with high-volume needs.
4. Where to Buy
Autoclaves can be purchased from a variety of sources:
Authorized Distributors: Check with the manufacturer's authorized distributors to ensure you are getting a genuine product with warranty and support.
Medical Equipment Suppliers: Many suppliers specializing in medical and laboratory equipment offer a range of autoclaves.
Online Retailers: Websites like Amazon or specialized equipment suppliers also offer autoclaves, but it’s important to check the credibility and warranty details before purchasing.
Some suppliers may also offer refurbished autoclaves at a lower price, which can be a cost-effective option if you are on a budget, but ensure they are fully serviced and certified before use.
12. Conclusion
Recap of Key Points
Pressure steam sterilizers, or autoclaves, are essential tools for ensuring the sterility of medical, dental, laboratory, and industrial materials. By using high-pressure steam to eliminate harmful microorganisms, these devices play a crucial role in various industries, from healthcare to food processing. Throughout this article, we’ve covered:
The history and evolution of autoclaves, showcasing how they’ve advanced in design and functionality.
The principles of steam sterilization, emphasizing the key factors—temperature, pressure, and time—that make steam an effective sterilizing agent.
A breakdown of the types of autoclaves, including gravity displacement, pre-vacuum, and SFPP models, each suited for different applications.
The sterilization process from preparation to monitoring and validation, ensuring that materials are safely and effectively sterilized.
The importance of maintenance and troubleshooting to ensure that autoclaves remain reliable and effective over time.
The regulatory standards that govern the use of autoclaves, such as FDA regulations, CDC guidelines, and ISO standards.
The recent innovations in autoclave technology, including advanced control systems, energy efficiency improvements, and connectivity features.
Key considerations when choosing the right autoclave, such as capacity, cycle time, and budget.
The Future of Steam Sterilization
As technology continues to evolve, so does the field of pressure steam sterilization. Looking ahead, we can expect even more advanced technologies and innovations aimed at improving sterilization processes:
Smart Autoclaves: With greater connectivity, autoclaves will continue to evolve into “smart” devices capable of real-time monitoring, remote operation, and enhanced data analytics. The integration of AI and machine learning could further streamline sterilization cycles, predicting maintenance needs and improving efficiency.
Sustainability: As environmental concerns grow, autoclaves will likely see even more eco-friendly designs, including water-saving technologies and reduced energy consumption. The trend toward sustainability is expected to continue, with manufacturers focusing on creating low-emission, resource-efficient systems.
Customization: Future autoclaves will likely offer even greater customization options for different types of sterilization loads. From tailored cycle settings to advanced software that can handle complex sterilization tasks, customization will be key for meeting the specific needs of various industries.
Final Thoughts
Pressure steam sterilizers are indispensable tools in ensuring the safety and sterility of equipment, materials, and consumables across a wide range of industries. Choosing the right autoclave requires careful consideration of your facility’s unique needs, budget, and the type of materials you need to sterilize. By understanding the latest innovations, adhering to regulatory standards, and maintaining your equipment properly, you can ensure that your autoclave operates at peak efficiency and continues to provide reliable performance for years to come.
As the sterilization industry continues to evolve, staying informed about the latest technologies and best practices will help you make the best decisions for your sterilization needs, ultimately ensuring a safer, cleaner, and more efficient environment.

 English
English русский
русский Français
Français Español
Español bahasa Indonesia
bahasa Indonesia Deutsch
Deutsch عربى
عربى 中文简体
中文简体