Safety Management of High-Pressure Sterilization Equipment in Disinfection Center
Posted by Admin | 28 Nov

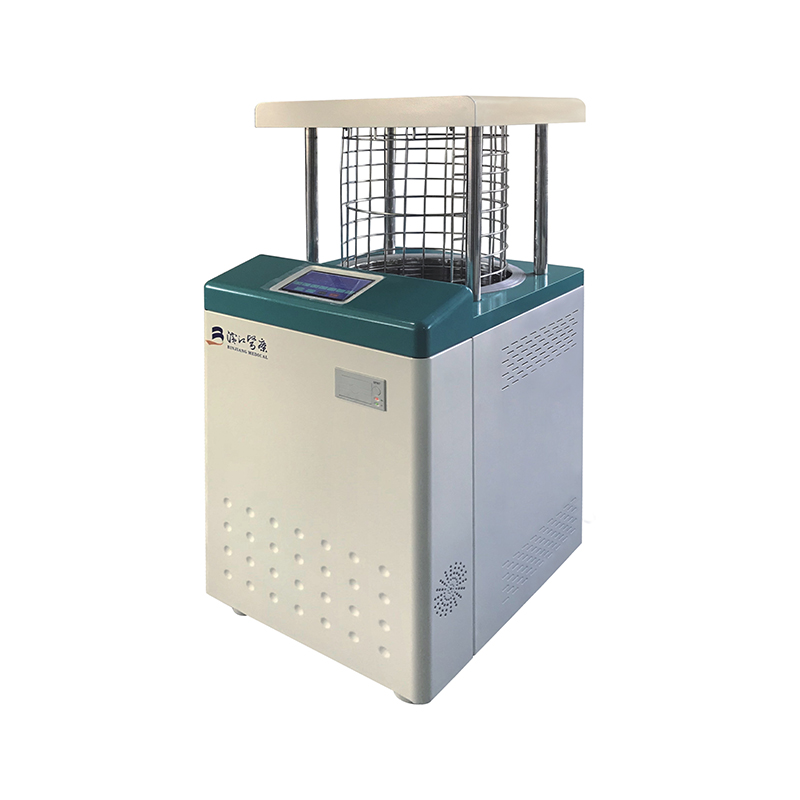
With the development of medical technology, hospitals have placed higher demands on the work of their central sterilization supply rooms (CSS). The CSS has transformed from an auxiliary department into a crucial department for controlling nosocomial infections. Ensuring the sterilization quality of sterilized items is a vital aspect of controlling nosocomial infections. High-temperature, high-pressure steam sterilization is a widely used technique in CSS of large and medium-sized hospitals. However, high-temperature, high-pressure steam sterilizers are containers under key national monitoring. Proper management, correct operation, and regular testing and maintenance are essential for the safe operation of the equipment and ensuring the quality of sterilization. The following is a report on our hospital's experience in the maintenance and performance upkeep of pressure sterilizers.
1. Qualification Certification of Sterilization Personnel
Strengthen professional training for sterilization personnel, ensuring they are certified before starting work. They should possess knowledge of disinfection, sterilization, and microbiology, including understanding the working principles, operation, maintenance, and troubleshooting of sterilizers; requirements for the placement and loading of relevant items; monitoring methods for sterilizers; the setting requirements for bioindicator monitoring of high-pressure steam sterilizers; and methods for placing monitored items. Strict adherence to operating procedures is required. Personnel must not leave their posts during working hours, demonstrating a strong sense of responsibility and diligence to prevent errors and accidents, thereby improving work efficiency and professional competence.
2. Safe Operation
2.1 Daily Maintenance
Sterilization personnel must understand the basic principles of the pressure sterilizer, the performance and uses of safety accessories (safety valves, pressure reducing valves, various valves, pressure gauges, liquid level gauges, thermometers), and be proficient in the equipment's performance, operating methods, and daily maintenance.
2.1.1 Before daily use, flush the exhaust port, check for unobstructed exhaust, and clean the exhaust filter to remove debris. Perform dust removal on the sterilizer by wiping the inner wall and inner carriage with clean water, keeping the pressure steam sterilizer's inner wall and inner carriage clean and dry before use. Check the sealing rings and safety locks for proper function. Check that the water source and air compressor supply reach the specified pressure; only when the pressure is qualified can the power supply and sterilizer control switch be turned on for preheating.
2.1.2 Use the color change of the B-D test strips to determine if there is residual cold air in the sterilizer, ensuring normal sterilization can proceed.
2.2 Regular Maintenance
Pull the safety valve several times a week while the jacket is pressurized to ensure it functions properly. Scale buildup can obstruct steam conduction; therefore, spray a scale remover evenly onto the inner wall of the sterilizer weekly, once the internal wall temperature has dropped to 25-30°C. After 10 minutes, wipe the scale off with a cotton cloth. This prevents scale buildup on the inner wall of the pressure steam sterilizer from hindering steam conduction and preventing normal heat release.
Remove the sealing ring monthly, clean it, dry it, apply silicone oil, and then reinstall it to prevent slippage.
Quarterly, have medical engineering personnel perform maintenance and inspection on the inner carriage of the sterilizer to ensure smooth steering, inspect the steam generator, replace sealing rings, and remove scale from the heating elements to ensure safe operation of the equipment.
Under high temperature and pressure, the safety devices of autoclaves may malfunction, fail, corrode, become clogged, or leak. According to relevant national standards and specifications, the equipment safety inspection period is clearly defined. Each year, personnel from the Medical Engineering Laboratory should regularly disassemble various safety valves and have them inspected by the relevant department. If a sterilizer malfunctions and the sterilization personnel cannot handle it themselves, they should report the problem through the equipment maintenance network established by the Medical Engineering Laboratory, and a designated professional engineer will repair the fault.
3. Quality Management of Sterilization Packages
The quality of the inside and outside of the package before sterilization directly affects the sterilization effect. Therefore, quality management of the items to be sterilized should be strengthened to ensure the sterilization effect. Factors such as excessively large, tight, or loose packaging, and the breathability and cleanliness of the packaging material will affect the removal of cold air and the penetration of water vapor. Reusable fabrics should be collected, cleaned, and treated before reuse. Boxes, plates, and bowls should be individually packaged whenever possible. Package sizes should not exceed 30cm × 30cm × 50cm. Dressing packages should not exceed 5kg, and instrument packages should not exceed 7kg. Instrument trays should use perforated bases to facilitate steam penetration and prevent wet packaging. Each package should have chemical indicator tape on the outside and a chemical indicator card inside.
4. Establish Management Systems
Establish and improve rules and operating procedures. Only by establishing strict work systems can we ensure that there are rules to follow, guaranteeing work quality and final quality. Sterilization personnel must be certified and strictly implement all work systems and operating procedures. During high-pressure steam sterilization, sterilization personnel must strictly control the pressure, temperature, and time according to the type of items and instruments to ensure sterilization quality. They must also conduct safety checks before and after sterilization and promptly notify the medical engineering department for repair in case of malfunctions. Operation with malfunctions is prohibited. The head nurse and quality control personnel should regularly check the implementation of various systems and operating procedures by sterilization personnel and provide rewards or penalties accordingly.
5 Lessons Learned
Ensuring the quality of sterilized items and strictly adhering to disinfection technical specifications are crucial. Establishing and improving a sterilization monitoring system, enhancing the professional skills of operators through specialized training, requiring sterilization personnel to hold sterilization operator certifications, being familiar with the function of each part of the sterilizer, conducting routine pre-sterilization checks, strictly following operating procedures during sterilization, constantly monitoring changes in components, and promptly addressing any abnormalities are all essential to ensuring sterilization quality and effectively controlling and preventing hospital-acquired infections.

 English
English русский
русский Français
Français Español
Español bahasa Indonesia
bahasa Indonesia Deutsch
Deutsch عربى
عربى 中文简体
中文简体