Veterinary-Use Sterilizer Selection & SOPs
Posted by Admin | 09 Nov
Why a veterinary-use sterilizer is different
Veterinary clinics process a wider variety of items than many human clinics: surgical instruments sized for different species, implantable devices, endoscopes, bandaging tools, and porous materials such as towels and gowns. A veterinary-use sterilizer must accommodate diverse loads, tolerate heavier soil and organic matter, and support reliable routine monitoring and record-keeping. Choosing the right sterilizer and implementing correct procedures reduces post-operative infection, protects staff, and ensures regulatory compliance.
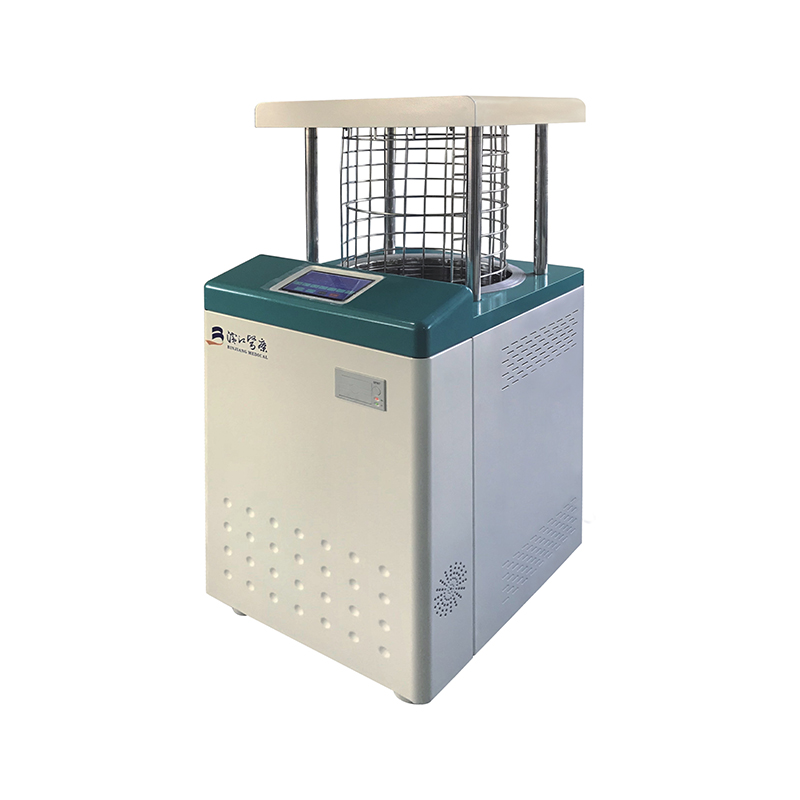
Types of sterilizers used in veterinary practice
Understanding strengths and limits of each technology helps you match clinic needs to practical performance and budget.
Steam autoclaves (gravity and pre-vacuum)
Steam autoclaves are the workhorse for most veterinary clinics. They reliably sterilize wrapped instruments, textiles, and many implants. Pre-vacuum (vacuum-assisted) autoclaves remove air before steam penetration and are better for wrapped loads and hollow instruments. Gravity autoclaves are simpler and cheaper but require careful loading to avoid cold spots.
Dry heat sterilizers
Dry heat is suitable for items that tolerate high temperatures but must remain dry (e.g., some oils, powders, and non-aqueous materials). Dry heat requires higher temperatures and longer exposures than steam and is less energy-efficient for large loads.
Chemical sterilization (ETO, hydrogen peroxide, peracetic acid)
Gas or low-temperature liquid sterilants are used for heat-sensitive items such as certain endoscopes and electronics. Ethylene oxide (ETO) is effective but requires long aeration times and regulatory controls. Low-temperature hydrogen peroxide and peracetic acid systems offer faster cycles and are increasingly popular for delicate instruments.
Key selection criteria for clinics
When selecting a veterinary sterilizer, weigh capacity, cycle types, throughput needs, footprint, and consumable costs. Consider the patient load, common procedures (soft tissue vs orthopedic), and whether you need validated cycles for implants.
- Capacity: Chamber size and rack configuration to handle trays, bowls, and cassettes used for different species.
- Cycle variety: Ability to run wrapped, unwrapped, porous, and hollow instrument cycles (and low-temperature cycles if needed).
- Validation/monitoring compatibility: Biological indicators, chemical integrators, and data-log export for QA.
- Maintenance and service: Local technical support and warranty, plus ease of routine maintenance.
- Safety features: Door interlocks, pressure/temperature fail-safes, and exhaust treatment for chemical systems.
Practical sterilization cycles and parameters
Below are commonly used target parameters. Always follow the sterilizer manufacturer's validated cycle data and the instrument/case manufacturer's recommendations for implantable items.
| Load type | Method | Typical parameters | Notes |
| Wrapped surgical instruments | Pre-vacuum steam | 134°C for 3–4 min (sterilization phase) | Shorter exposures at higher temp if validated; allow drying time. |
| Porous loads (towels, gowns) | Gravity or pre-vacuum steam | 121°C for 15–30 min | Ensure proper packaging and steam penetration. |
| Hollow instruments, lumens | Pre-vacuum steam or specialized low-temp system | Pre-vacuum 134°C, adjusted exposure per validation | Use lumen connectors and validated cycles. |
| Heat-sensitive electronics | Hydrogen peroxide or peracetic acid low-temp | Manufacturer cycle (e.g., 50–60°C equivalent low-temp) | Follow device manufacturer guidance and aeration steps. |
Sterilizer validation and routine monitoring
Validation and ongoing monitoring are mandatory quality controls. Use a combination of mechanical (printouts/data logs), chemical (process indicators and integrators), and biological indicators (BIs) to confirm sterility assurance levels. For implantable devices or high-risk procedures, run biological indicators on a weekly basis or per local regulation.
- Mechanical: Record cycle temperature, pressure, vacuum, and cycle time; keep logs for audits.
- Chemical: Use external indicators on every pack and internal integrators inside representative packs.
- Biological: Incubate BIs and document results; investigate any failures immediately.
SOP checklist for daily sterilizer operation
A clear, accessible SOP reduces user error and ensures consistent outcomes. The checklist below should be adapted to your clinic's equipment and local regulations.
- Pre-clean and inspect instruments: ultrasonic cleaning, manual brushing, and visual inspection for bioburden.
- Load correctly: do not overcrowd; orient lumens and hinges for steam access; wrap per validated methods.
- Select validated cycle and start data logging; place internal integrator in representative pack.
- Dry and cool: ensure packs are dry before storage to prevent contamination and corrosion.
- Label and document: cycle ID, operator, date/time, load contents, and BI/integrator results.
Maintenance, troubleshooting, and safety
Regular preventive maintenance extends equipment life and prevents cycle failures. Train staff on common troubleshooting steps and emergency procedures for chemical sterilizers. Always use PPE when handling BIs, chemicals, and hot loads, and ensure vents and exhausts are properly routed.
Common problems and fixes
- Failed biological indicator: Quarantine batch, repeat process, review cleaning and loading, contact service if mechanical issues suspected.
- Poor drying: Review cycle selection, check vacuum and drain systems, reduce load density and improve packaging.
- Unusual noises or leaks: Stop cycle, isolate equipment, and call certified technician; do not attempt major repairs in-house.
Recordkeeping and regulatory considerations
Keep sterilization records for the period required by local veterinary boards or health authorities. Include cycle prints/logs, BI results, maintenance logs, operator training records, and corrective actions. For clinics that perform implant surgeries, maintain traceability of implant lots to sterilization records and patient files.
Final recommendations
Select a sterilizer that matches your clinic’s throughput and instrument mix, prioritize pre-vacuum steam or validated low-temp systems for complex loads, implement written SOPs and monitoring programs, and establish routine maintenance and training. Investing in correct sterilization practice protects patients, staff, and the clinic’s reputation.

 English
English русский
русский Français
Français Español
Español bahasa Indonesia
bahasa Indonesia Deutsch
Deutsch عربى
عربى 中文简体
中文简体